Osteochondrosis (degenerative disks disease) in the lumbar spine or lower back is due to involutionary changes in discs, which leads to lower back pain.
Intervertebral discs are tough, fibrous structures that act as ligaments between vertebrae, absorbing shock and providing shock absorption to the spine.The discs are flexible but strong enough to facilitate movements such as bending your torso forward, backward or sideways.
Despite the name, osteochondrosis is not considered a true disease and symptoms over time, as a rule, does not worsen.Disks, as well as all structures of the body, degrade, and disk degeneration develops in all people, as part of the involutionary process.
A characteristic feature of osteochondrosis is a gradual decrease in symptoms as the spine begins to stabilize.Treatment of osteochondrosis of the lumbar spine is focused on minimizing pain, stabilizing the spine and improving or maintaining mobility.
Symptoms

Most cases of manifestation of osteochondrosis of the lumbar spine are to have a slight, constant back pain, which from time to time intensifies for several days or more.
Symptoms may vary, but the most characteristic include:
- Moderate, constant lower back pain.Pain in the damaged disk are the most common symptom of disk degeneration.The pain can spread to the buttocks, groin and upper thigh.This pain is usually felt as dumb, and the intensity can vary from light to severe.
- Periodic acute episodes of pain.The back pain can be intensified for several days or weeks, and then return to a more moderate level.Outbreaks of pain occur as degeneration and subside as the spine is gradually stabilizing.Outbreaks of pain can occur suddenly and pain manifestations often lead to a decrease in mobility.
- Local soreness.The lower part of the back surrounding the degenerated disc can be sensitive to touch.Local pain is caused by inflammation and muscle tension in the area of the disk damaged by degeneration.
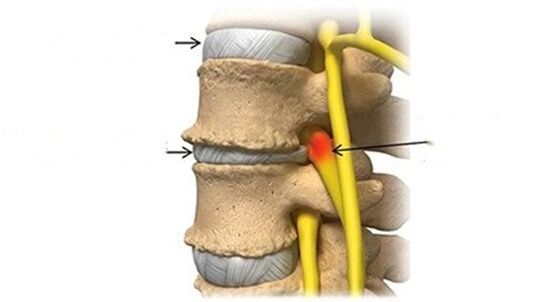
- Pain in the leg.Neurological symptoms, including numbness, weakness or sharp, shooting pain in the buttocks, hips and / or back of the leg, can be felt if the height of the disk is significantly reduced, and the conditions for compression of the nerve root arise.The pain in the legs with osteochondrosis of the lumbar spine usually does not fall below the knee.
- A sense of sudden weakness or instability can occur with a significant weakening of the disk and the patient creates that the lower back is incompletely performing its functions.
In addition, the pain may intensify or decrease when performing some movements or certain poses, such as:
- Pain in the seat.Sitting over long periods often causes increased lower back pain and stiffness and decreases after arising or change of position.
- Strengthening pain with tilting or rotation.Twisting the spine and tilt forward, back or side can cause intense, pain in the damaged disk.
- Reducing pain when walking or changing position.When the spine changes the position, the pressure on the discs decreases or is redistributed from discs to muscles and joints.Frequent positions, alternating standing and sitting, as well as short walks can help reduce stiffness and minimize pain.
Disk degeneration should not cause symptoms of intestinal dysfunction / bladder, fever with back pain, inexplicable and rapid weight loss or intensive abdominal pain.These symptoms indicate more serious conditions and often require operational methods of treatment.
Associated symptoms
With osteochondrosis of the lumbar spine, in addition to the lower back pain, other symptoms associated with disk degeneration may occur.For example:
- Proteins contained inside the disk can cause significant inflammation if they come into contact with the surrounding spinal structures, and this inflammation can lead to spasms of the lower back muscles, as well as radial pain, with radiation in the hips and on the posterior surface of the lower extremities (also called Ishias).
- Degeneration of the lumbar disk can contribute to the development of lumbar stenosis and / or lumbar osteoarthritis, as well as other conditions in the lower back.
- A degenerated disk can also lead to the appearance of a hernia of the lumbar intervertebral disc.Neurological symptoms with a hernia of a disk can be acute and intense.
- The symptoms caused by the degeneration of the disk in the lumbar spine can vary widely depending on how quickly or completely the disk has undergone degeneration and how it affects the surrounding spinal structures.
- Pain for osteochondrosis is usually caused by deformation of the muscles that support the spine and inflammation around the structures nearby to the disc.
Causes of osteochondrosis of the lumbar spine
Osteochondrosis occurs due to age-related wear and tear of the disc structure, and the degeneration process can be accelerated by injury, general condition, health and lifestyle, and possibly a genetic predisposition to the development of pathological processes in the musculoskeletal system.
Osteochondrosis rarely begins with a serious injury, such as a car accident.It is more likely that the initiation of degenerative processes is associated with low-energy disc trauma.
Law pain associated with lumbar osteochondrosis are usually generated by one or more pathological processes:
- Inflammation, proteins from the disk are irritated by the surrounding nerves - both small nerves in the disk itself and potentially large nerves that go to the feet (sciatic nerve).
- The abnormal instability of the micro, when the outer rings of the disk, called the fibrous ring, wear out and cannot effectively absorb power vectors on the spine, which leads to movements along the vertebral segment.
- For a long period of time, the pain in osteochondrosis of the lumbar spine ultimately decreases, and not gets worse.This relief of pain occurs because the disk completely damaged by degeneration no longer has any inflammatory proteins (which can cause pain) and the sleeping disk passes into a stable position, eliminating micro-movements that cause pain.
Risk factors
Life lifestyle factors that affect the general state of health can affect intervertebral discs.The risk factors of a degenerative disk disease (osteochondrosis) include:
- Family history of back pain or skeletal and muscle disorders
- Excessive load on the bottom of the back, due to playing sports, or the nature of the work
- Long static loads on the discs due to prolonged seats and / or poor posture
- Lack of disks support due to weak back muscles
- Obesity
- Smoking or any form of consumption of nicotine
Disk degeneration is part of the aging of the body, but not all people develop pain or any special symptoms.Symptoms tend to occur in case of instability, muscle tension and, possibly, irritation of the nerve root.
Diagnostics
- The history of the disease includes a detailed study of the symptoms in the patient, their intensity and the relationship of pain with the loads or position of the body.Information about regular physical activity, sleep habits and past injuries is also needed.
- A physical examination is necessary to study the range of movements and the state of the muscle corset.The presence of painful areas on palpation or physical abnormalities is also determined.In addition, neurological tests are carried out to determine a neurological deficit.
- The above diagnostic methods are usually sufficient for the diagnosis of osteochondrosis, but an accurate diagnosis requires the use of visualization methods.
- Ct
- Radiography
- MSCT
- PAT
- MRI - this diagnostic method allows you to clarify the degree of degeneration, the presence of fractures, hernias of stenosis discs.Often an MRI study is necessary in preparation for surgical treatment in order to accurately determine the location of the degenerated disk and plan the operation.

Studies have shown that the results of MRI with moderate or significant disks degeneration are found when scanning patients, both with severe pain and minimal or lack of pain.In addition, many painful conditions may not appear on an MRI.For this reason, the diagnosis cannot be made exclusively on the basis of the results of visualization, and verification of the diagnosis is possible only on the basis of the totality of all clinical and instrumental examination methods.
Treatment
The initial methods of treating osteochondrosis of the lumbar spine and pain manifestations usually include the following combinations:
- Overcomplex painkillers They can reduce inflammation, which contributes to discomfort, stiffness and irritation of nerve roots.
- Prescription painkillers.In severe pain, muscle relaxants or narcotic painkillers can be prescribed.These drugs are usually used to treat intensive, acute pain, which is expected to last more than a few days or weeks.These drugs can cause addiction and cause serious side effects, so they should be used with caution.
- Heat and ice.The use of heat in the lower back improves blood circulation, which reduces muscle cramps and tension and improves mobility.Ice packages can reduce inflammation and relieve moderate pain.It is useful to use heat before physical exercises to relax muscles and use ice after physical activity in order to minimize inflammation.
- Manual therapy. The manipulation of which is carried out by a specialist is a popular method of control of pain in lower back pain.Practicing doctors, manual therapists, use their hands to influence various areas of the body in order to reduce tension in muscles and joints.It was found that manipulations are an effective measure for temporary pain reducing, and in some cases it is as effective as drug therapy.
- Massage.Exposure by massage methods can reduce tension and cramps in the muscles of the lower back, reduce pressure on the spine and relieve pain.In addition, therapeutic massage can improve blood circulation, ensuring the delivery of nutrients and oxygen to tense muscles.
- Epidural injections of steroids.The introduction of steroid into the space surrounding the spine can reduce pain impulses, as well as inflammation.Injection of steroid can be used in combination with the physical therapy program to relieve pain during physical exercises and rehabilitation.As a rule, the epidural injection of steroids allows to reduce pain by a period of several weeks to one year.
In many cases, for effective anesthesia, a combination of treatment methods is needed.The process of trial and error, as a rule, is necessary in order to choose a treatment that turns out to be the most effective.
Long bed rest is not recommended, and, as a rule, immobilization is possible with severe pain for a short period of time, since the lack of physical activity can lead to weakening of the muscles and normal support of the spine.
Exercise therapy and modification of activity

To maintain healthy mobility of the spine, physical exercises are needed.An effective exercise program for the lumbar spine should include:
- Stretching exercises for the muscles of the lower back, hips and pelvis, as well as the harmstring muscles.Tightening of these muscles increases pressure on the lumbar spine and contributes to the development of lower back pain.
- Power exercises on the muscles of the lower back and abdomen allow you to maintain good posture and it is better to maintain the spine.The program of exercises to strengthen muscles may include an individual exercise therapy program, dynamic stabilization of the lumbar spine, tai-chi, Pilates or others.
- Aerobic exercises with a low level of load, which increase the frequency of heart contractions, improve blood circulation and provide nutrients and oxygen, which is necessary to restore body tissues.For example, it can be walking, swimming and water aerobics.
Programs of physical exercises are usually adapted in each case, depending on the general state of health, the severity of pain and personal preferences.
In addition, small adjustments to everyday activity (modification of lifestyle) can effectively soften the pain.For example, dressing a corset when lifting weights or avoiding twisting when lifting weights, can prevent increased pain due to excessive loads on the discs.The use of an ergonomic chair and an orthopedic mattress can also improve posture and reduce the load on the discs.
Surgical treatment
Surgical treatment of osteochondrosis of the lumbar spine is necessary in cases where conservative treatment for 6 months was inefficient.Surgical treatment for osteochondrosis is always selective, which means that the patient himself decides whether the operation should undergo or not.
It is recommended to take into account all factors before deciding on an operation for osteochondrosis, including the duration of the recovery period, treatment of pain during recovery, and rehabilitation of the spine.
The mergers of the vertebrae
The standard surgical treatment for lumbar spine degenerative disc disease is fusion surgery, in which two vertebrae are fused together.The purpose of fusion surgery (spinal fusion) is to reduce pain and eliminate instability in the motion segment of the spine.
All spinal fusion operations are as follows:
- The damaged disk is completely removed from the intervertebral space (discoctomy).
- Stabilization is carried out using a bone transplant and / or tools (implants, plates, rods and / or screws).
- Then the vertebrae fuse, forming a solid, motionless structure.Fighting occurs within several months after the procedure, and not during the operation itself.
After the operation, wearing a corset, taking analgesics are prescribed.Exercises are connected very carefully, taking into account the individual characteristics of the patient and the degree of tissue regeneration.Complete recovery after the merger may take up to a year until the vertebrae is growing together.
Surgical replacement of an artificial disc
Replacing the damaged disk with an artificial implant has been developed in recent years as an alternative to mergers.The disk replacement operation consists in completely removing the disk damaged by degeneration (discoctomy), the restoration of disk space to the natural height and the implantation of the artificial disk.
This procedure is designed to maintain movement in the spine similar to natural movements, reducing the likelihood of increasing pressure on neighboring spinal segments (fairly common complication of spinal fusion).
Recovery after the disk replacement operation usually lasts up to 6 months.






















